Grieving Bulimia: When Self-Destruction Hides Behind a Smile
Grief with bulimia is hidden in plain sight, smiling through dinners, hiding tears in bathrooms, and watching someone lose themselves in silence.

This post blends real grief with grounded knowledge. It isn’t clinical. It isn’t distant. It’s meant to sit beside you—not above you. The story you’ll read is meant to reflect what so many feel when living through or witnessing this condition: confusion, exhaustion, and quiet forms of courage.
If what you read feels familiar, please speak with your doctor. Your pain deserves more than silence.
She Said She Was Fine with Her Lips, but Not with Her Eyes
I never used to count things…at least not in the ways people often caution you about like calories or steps.
But I did count the seconds between the waves that rose in my throat before I caved. I remember convincing myself that I was just tired, maybe a little sick, or that I simply didn’t want to be around food at all. Then, I started taking pictures of myself on the bathroom scale as proof that something was leaving me, that I was getting lighter.
But really, I wasn’t…not in the way that truly mattered.
🧠 Symptoms:
- Binge episodes: Eating unusually large amounts of food in short periods, often in secret
- Loss of control during eating, followed by distress or guilt
- Purging behaviors: Vomiting, over-exercising, or misuse of laxatives, diuretics, or enemas
- Restrictive behavior between binges: Skipping meals, fasting, or cutting out entire food groups
- Body image disturbance: Self-worth based on weight or appearance
- Mood swings, anxiety, and obsessive thoughts about food and body
- Physical signs: Swollen cheeks, dental erosion, knuckle calluses, acid reflux, weight fluctuations
It always began with something insignificant, like cereal or pasta—something I assured myself I could handle just this once; then I’d snap, devour everything, and hate myself so quickly that it felt like whiplash.
It was as if I blacked out in the kitchen only to wake up on the bathroom floor, clinging to the edge of the toilet like it was a lifeline. I recall a moment when I gagged and spotted a piece of corn, relief washed over me; it was still whole, and that somehow meant I was doing it right, getting it out before it lingered too long and became part of me.
People often assume it’s about vanity, control, or a desire to be thin. But it isn’t always that simple. Sometimes it’s about wanting to disappear without dying. Sometimes it’s about hating your mouth so much that you punish it for ever craving anything.
Complications:
- Electrolyte imbalances: Can cause irregular heartbeat, heart failure
- Dehydration & kidney failure
- Gastrointestinal damage: Esophageal tears, stomach rupture, rectal prolapse
- Tooth decay & gum disease
- Hormonal disruption: Missed periods, infertility
- Mental health deterioration: Self-harm, suicidal thoughts or actions
- Social withdrawal and emotional isolation
Causes:
- Genetic predisposition: Family history of eating disorders
- Psychological factors: Anxiety, depression, low self-esteem, trauma
- Environmental influences: Societal pressure to be thin, media ideals, bullying
- Dieting behavior: Severe restriction can trigger binge-purge cycles
It can be about drowning out the noise and seeking silence between bites and flushes JUST to find a sense of peace.
I became skilled at lying… I would claim I was just tired, that I had already eaten, or that I was doing a cleanse, or feeling unwell, or dealing with a headache. Anything to keep them from noticing the tremor in my hands after the fourth round, or the way I flinched when someone said “dinner,” as if it were a threat.
The worst part wasn’t the vomiting; it was the shame that always followed, Shame was always louder, It sat with me on the bathroom tiles, whispering that I’d never be enough, no matter how empty I made myself. I could vomit until blood came up, and I’d still feel full of everything I couldn’t fix.
Even now, I can present myself as normal, I say the right things and act the right way, but the voice remains; It’s just quieter now, waiting longer between rounds.
Sometimes, I still skip meals, not to lose weight, but to prove to myself that I can say no. It’s a way to remind myself that I’m not that girl anymore.
Yet, the truth is… I am… She’s just quieter now, too. And on some days, I find myself missing her. She made me feel powerful, if only for about twenty seconds before the shame pulled me back under.
I traded hunger for silence—and silence for shame. I never came out whole
Risk Factors:
- Age & gender: Most common in females, often begins in late teens or early adulthood
- Mental health conditions: Especially mood disorders, anxiety, or substance use
- Personality traits: Perfectionism, impulsivity, sensitivity to criticism
- History of trauma or abuse
- Participation in weight-focused environments (e.g., athletics, dance, modeling)
📘 Diagnosis & Treatment
Diagnosis:
- Clinical interview: Focus on eating behaviors, body image, and emotional health
- Physical exam: Look for signs of malnutrition, dehydration, or physical damage from purging
- Lab tests: Assess electrolyte levels, kidney function, and heart health
- Mental health assessment: May include screening for co-occurring conditions
- Diagnosis typically requires binge-purge behavior at least once a week for 3 months—but any level of disordered behavior warrants care
Treatment:
- Psychotherapy:
CBT-E (Enhanced Cognitive Behavioral Therapy): Gold standard; targets core beliefs and behaviors - Family-Based Therapy (FBT): Especially effective for teens; empowers parents to support recovery
- Dialectical Behavior Therapy (DBT): Builds emotional regulation and interpersonal skills
- Medications:
Fluoxetine (Prozac): Only FDA-approved medication for bulimia; reduces binge/purge frequency - May also address co-occurring depression or anxiety
- Nutritional Rehabilitation:
Registered dietitians create structured meal plans and reintroduce balanced eating - Focus on ending restriction, normalizing food intake, and repairing hunger cues
- Hospitalization:
Needed for severe symptoms, medical instability, or mental health crises - May include inpatient, residential, or day-treatment programs
- Lifestyle Support & Prevention:
Avoid labeling foods as “good” or “bad”
Continued:
- Discourage dieting and body-shaming language at home
- Promote media literacy and self-worth outside of appearance
- Encourage regular family meals and open conversations about food and emotions
- Self-Care and Coping:
Follow your care plan: Attend all sessions and complete at-home work - Reduce body-checking behaviors: Avoid mirrors, scales, or excessive comparisons
- Watch for relapse signs: Stress, life transitions, or skipped meals can trigger old patterns
- Seek support: Trusted friends, support groups, or family involvement help maintain healing
I know this is heavy, and I understand that the road ahead may feel like a tangle of loss and unanswered questions. But please hear this: you are not broken because you are hurting; you are not weak because you are afraid. You are living through something real, and survival itself is a kind of grace. You are allowed to struggle, you are allowed to hope, and you are allowed to not have all the answers today. Whatever comes next, you do not face it empty-handed; you carry every moment of love that shaped you, and that will always be enough to keep going.
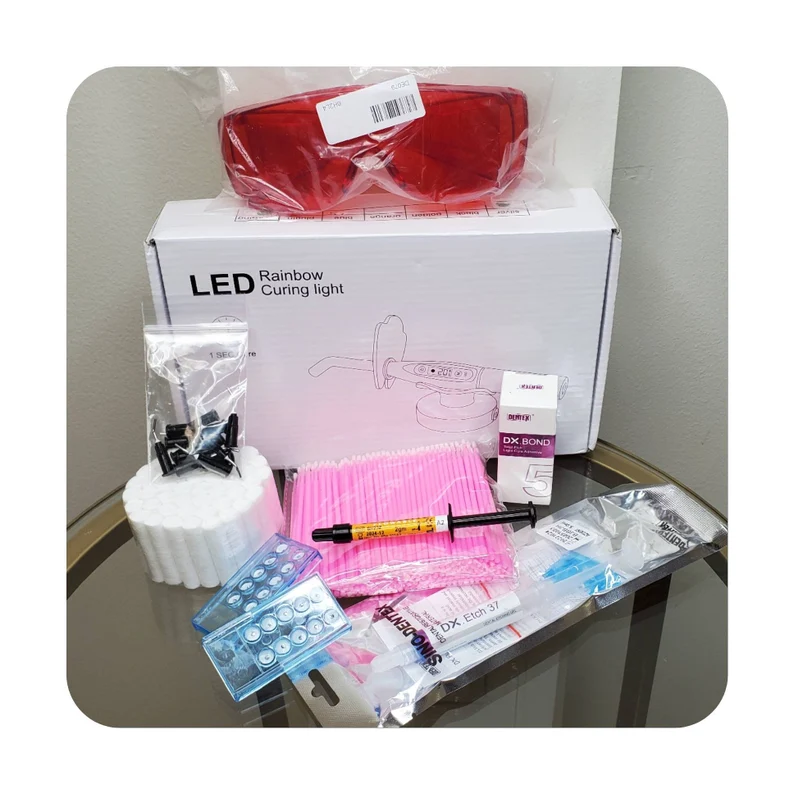
🎀 Gifts to help With Bulimia
🏥 Everyday Comforts for Everyday Battles
Managing Bulimia often means needing a little extra help.
Sometimes it’s about restoring dignity, ease, or simply getting through the day with less pain.
These carefully chosen tools aren’t just items; they’re small bridges back to living.
This section is about finding practical support, never shame.
DIY Tooth Gem Kit – If You’re Gonna Hurt Your Teeth, At Least Make Them Shine
Bulimia steals so much, control, peace, enamel. If the cycle hasn’t stopped, but the mask still needs fixing, this DIY tooth gem kit offers a strange kind of glittering defiance. It’s not a solution. It won’t save your smile. But it might let you reclaim one small choice in a body that feels out of control. Beauty in the ruins. Shine on, even if you’re still breaking.
🌿 Paths to Healing Beyond the Map
Sometimes traditional medicine isn’t enough.
If you’re exploring gentle, alternative options to help with Bulimia,
you might find comfort in plant-based compounds like **CBD or CBG**.
*This section is not medical advice, just a door left open.*
USA Medical Stress Relief Total Pack – Support for the Storm Behind the Behavior
Binging and purging are not about appetite, they’re about trying to silence what’s screaming inside. This Total Pack blends broad-spectrum CBD with calming adaptogens and mood support to help reduce anxiety, emotional volatility, and panic spirals. It’s not treatment. But it can be a companion to therapy—a gentle aid for the quiet hours when everything feels too loud.
Need a Different Path Forward?
Every journey through grief looks different. Choose the next step that speaks to where you are now:
When You're Ready to Start Healing
Healing doesn’t mean forgetting.
It means finding small ways to carry your grief with strength and grace.
These are the stories, tools, and gentle steps to begin walking forward…at your own pace.
When You're Still in the Thick of It
Sometimes healing feels like a lie.
If you’re not ready to move on…if the pain still roars louder than the world wants to hear…this is the place where you’re allowed to feel it.
No sugarcoating. No pretending. Just truth.
When You're Holding on to Who’s Still Here
Grief reminds us to love louder.
If someone you love is still with you, this is your place to celebrate them, honor them, and create new memories while there’s still time.
Joy and sorrow can live side by side.