Grieving COPD: When Every Breath Becomes a Battle
Grief with COPD begins with shallow breaths and deep fear—watching someone you love struggle for air while their world slowly shrinks around them.
This post blends real grief with grounded knowledge. It isn’t clinical. It isn’t distant. It’s meant to sit beside you—not above you. The story you’ll read is meant to reflect what so many feel when living through or witnessing this condition: confusion, exhaustion, and quiet forms of courage.
If what you read feels familiar, please speak with your doctor. Your pain deserves more than silence.
I Could Hear His Lungs Losing the Fight
I could sense it before he even spoke… The wheeze, The pauses in his speech, The way his breath would falter mid-sentence as if the words themselves were too heavy to carry.
Once, his laughter filled the space around us, a booming, joyous sound that resonated deep within. But slowly, it started to fade away, like a distant echo. First, the laughter disappeared, then came the struggle with the stairs, followed by the short walks to the mailbox.
🧠 Symptoms:
– Shortness of breath, especially with exertion
– Chronic cough with mucus (clear, yellow, green, or white)
– Wheezing or whistling breath sounds
– Chest tightness
– Fatigue or low energy
– Recurrent respiratory infections
– Unintentional weight loss (in later stages)
– Swelling in ankles, feet, or legs
– Exacerbations: symptom flare-ups triggered by cold air, infections, or pollutants
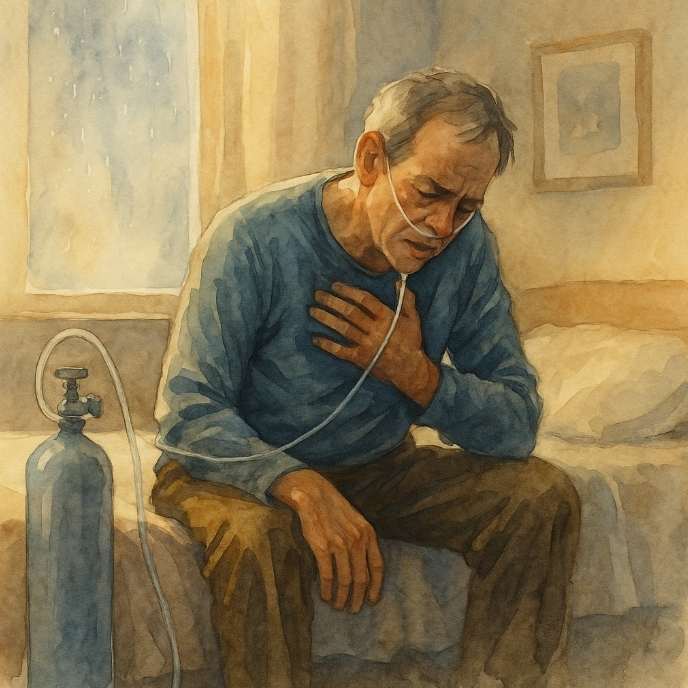
At first, he reassured me he was just tired, slightly winded, nothing too concerning. But the persistent cough never left, and one morning, I received a frantic call from him, sprawled on the kitchen floor, too dizzy to stand, gasping for air in a house that felt heavy with it.
They diagnosed him with COPD—Chronic Obstructive Pulmonary Disease. Three lengthy words that echoed a new reality: the world would never feel easy again.
He stopped smoking… He adhered to every guideline, the harm had already been done, ghosts lingered in his lungs, reminders of every puff he thought was insignificant.
The oxygen tank became part of our daily lives. He wheeled it behind him, a constant companion, hissing softly with every labored breath. He seldom ventured outside, losing trust in the air that once felt so fresh.
Complications:
– Respiratory infections (e.g., flu, pneumonia)
– Heart disease and arrhythmias
– Lung cancer
– Pulmonary hypertension
– Depression and anxiety
– Acute respiratory failure during exacerbations
Causes:
– Long-term exposure to lung irritants:
– Cigarette smoke (primary cause)
– Cigar and pipe smoke
– Air pollution
– Workplace exposure to dust, fumes, or chemicals
– Indoor smoke from cooking/heating (especially in homes with poor ventilation)
– Genetic condition: Alpha-1-antitrypsin deficiency (rare)
I learned a new term: “exacerbations” far too intimately. These flare-ups felt like drowning while still above water. In those moments of panic, the machine would blink and beep, both of us holding our breath, while he struggled to catch his.
He shared that the hardest part wasn’t the struggle for breath; it was how the world seemed to shrink around him. His life turned into a small existence with just four rooms, two inhalers, and a calendar filled with medical appointments.
Even on the brighter days, when he could sit by the window and share stories with me, I watched the rise and fall of his chest, like the gradual ticking of a clock winding down.
He never wished for extra time. Just a reprieve from the fear. Less gasping for air. Less pretending he didn’t long for the sound of his laughter.
He once said, “Breathing used to be something I did without thought. Now, it’s consumed my every thought.”
That’s the reality of COPD…it doesn’t rob you of life all at once. Instead, it forces you to savor every fleeting breath.
Preventions:
- Quit smoking: Most important step to prevent and slow COPD
- Protective gear in toxic work environments
- Vaccinations: Flu, pneumococcal, COVID-19, RSV
- Avoid triggers: Cold air, allergens, fumes
- Healthy lifestyle: Balanced diet, physical activity, weight control
- Living with COPD:
Monitor symptoms: Daily weight, oxygen levels, sputum changes - Plan ahead for flares: Emergency meds, hospital bags
- Mental health support: Depression and anxiety are common
- Social and spiritual support: Group therapy, faith practices, or counseling
Risk Factors:
– Smoking (active or secondhand exposure)
– Occupational exposure to fumes or dust
– Childhood respiratory infections
– Asthma or airway hyperresponsiveness
– Family history of COPD
– Older age
– Low socioeconomic status (linked to higher exposure and less care access)
He didn’t pass away gasping—he lived each day that way until silence became a kind of mercy.
📘 Diagnosis & Treatment
Diagnosis:
- Pulmonary function tests (spirometry): Measures airflow obstruction
- Imaging:
- Chest X-ray: Detects changes and rules out other conditions
- CT scan: Provides detailed lung images
- Arterial blood gases: Assesses oxygen/carbon dioxide balance
- Genetic testing: For suspected AAT deficiency
- Oxygen saturation tests and exercise tolerance assessments
Treatment:
Medications:
- Bronchodilators (e.g., albuterol, ipratropium): Relax airway muscles
- Inhaled corticosteroids: Reduce inflammation
- Combination inhalers: Blend long-acting bronchodilators and steroids
- Phosphodiesterase-4 inhibitors (e.g., roflumilast): For chronic bronchitis
- Oral steroids: Short-term use during exacerbations
- Theophylline: Low-cost option, requires blood monitoring
- Antibiotics: Treat or prevent infections during flares
- Devices:
Inhalers and nebulizers for medication delivery - BiPAP (noninvasive ventilation): May be used at home in severe cases
- Supplemental oxygen: Improves quality of life and survival
Therapies & Procedures:
Pulmonary rehabilitation:
- Exercise training
- Education
- Nutrition and psychological support
- Airway clearance techniques: Controlled coughing, hydration, humidifiers
- Surgical options (severe emphysema):
- Lung volume reduction surgery
- Endobronchial valve placement
- Bullectomy
- Lung transplant
I know this is heavy, and I understand that the road ahead may feel like a tangle of loss and unanswered questions. But please hear this: you are not broken because you are hurting; you are not weak because you are afraid. You are living through something real, and survival itself is a kind of grace. You are allowed to struggle, you are allowed to hope, and you are allowed to not have all the answers today. Whatever comes next, you do not face it empty-handed; you carry every moment of love that shaped you, and that will always be enough to keep going.
🎀 Gifts to help With Chronic Obstructive Pulmonary Disease
🏥 Everyday Comforts for Everyday Battles
Managing Chronic Obstructive Pulmonary Disease often means needing a little extra help.
Sometimes it’s about restoring dignity, ease, or simply getting through the day with less pain.
These carefully chosen tools aren’t just items; they’re small bridges back to living.
This section is about finding practical support, never shame.
Oxygen Tank Backpack – Hands-Free Freedom for Life With COPD
For those living with COPD, mobility often depends on oxygen. This padded, lightweight backpack is designed to carry M6 or B-size tanks securely, keeping oxygen close without tying up your hands or weighing you down. With adjustable straps and durable construction, it turns a medical necessity into something quietly wearable. For walks, errands, or just moving from room to room, it gives you back some freedom with every breath.
🌿 Paths to Healing Beyond the Map
Sometimes traditional medicine isn’t enough.
If you’re exploring gentle, alternative options to help with Chronic Obstructive Pulmonary Disease,
you might find comfort in plant-based compounds like **CBD or CBG**.
*This section is not medical advice, just a door left open.*
USA Medical Total Support Pack – Relief for the Body That Fights for Every Breath
Living with COPD means rationing energy, words, and motion. This Total Pack blends CBD, sleep aids, stress relief, and immunity support to help ease the broader symptoms that come with struggling lungs, fatigue, inflammation, and the emotional toll of breathlessness. It won’t restore lung function. But it may soften the panic, support rest, and offer a gentler daily rhythm when oxygen feels like a negotiation.
Need a Different Path Forward?
Every journey through grief looks different. Choose the next step that speaks to where you are now:
When You're Ready to Start Healing
Healing doesn’t mean forgetting.
It means finding small ways to carry your grief with strength and grace.
These are the stories, tools, and gentle steps to begin walking forward…at your own pace.
When You're Still in the Thick of It
Sometimes healing feels like a lie.
If you’re not ready to move on…if the pain still roars louder than the world wants to hear…this is the place where you’re allowed to feel it.
No sugarcoating. No pretending. Just truth.
When You're Holding on to Who’s Still Here
Grief reminds us to love louder.
If someone you love is still with you, this is your place to celebrate them, honor them, and create new memories while there’s still time.
Joy and sorrow can live side by side.