Grieving J-Pouch Surgery: Mourning What Was Lost to Survive
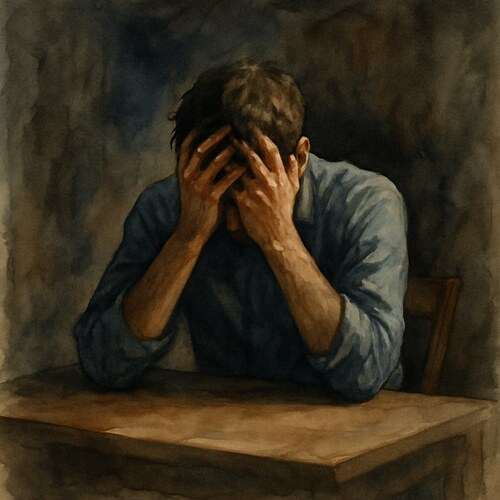
Grief after J-pouch surgery is complicated, relief shadowed by mourning for the body they had to sacrifice just to keep living.

This post blends real grief with grounded knowledge. It isn’t clinical. It isn’t distant. It’s meant to sit beside you—not above you. The story you’ll read is meant to reflect what so many feel when living through or witnessing this condition: confusion, exhaustion, and quiet forms of courage.
If what you read feels familiar, please speak with your doctor. Your pain deserves more than silence.
We Cheered for the Surgery but Grieved What It Cost
We believed the worst was behind us after the surgery.
Ulcerative colitis had already claimed so much…years filled with flares, hospital visits, urgent bathroom rushes, and nights spent curled up with a heating pad, cursing a body that refused to cooperate. So when the doctors proposed, “Let’s remove the colon and give you a J-pouch,” it felt like facing the final boss. Just one last battle, one last scar, and then perhaps, finally, peace.
We shed tears the day they wheeled him into the operating room. Hand in hand, we held on like people who believed in resolutions, the kind that heal, the kind that last.
When he woke up, groggy and stitched together but filled with hope, we celebrated. No more steroids. No more flares. No more war raging within his gut.
Yet, peace didn’t linger.
🧠 Symptoms:
– Diarrhea
– Belly pain and cramping
– Joint pain
– Fever
– Increased stool frequency
– Nighttime stool leakage
– Urgency or trouble controlling stool
A few months later, the symptoms began to creep back—urgency, cramps, that familiar hollow ache behind his belly button. He insisted it couldn’t be happening again. Maybe it was something he had eaten. Or maybe his body just needed more time to adjust.
But deep down, we both understood.
They called it Pouchitis—an inflammation of the J-pouch. It was common and treatable; nothing to panic about…at least, not yet.
Antibiotics were prescribed. He felt better…for a while.
But soon enough, the cycle emerged: symptom, pill, relief, repeat. Some days, the medications didn’t kick in quickly enough. Some weeks, they didn’t work at all.
He found himself measuring life by how close the bathroom was, once again mapping out exits in restaurants, canceling plans “just in case.”
Risk Factors:
– Having inflammatory bowel disease (especially ulcerative colitis)
– Regular use of NSAIDs (e.g., ibuprofen, naproxen)
– History of pelvic radiation therapy
He thought he’d crossed the finish line, but some diseases redraw the map while you’re still catching your breath.
Causes:
– Exact cause unknown
– Likely involves abnormal interaction between gut bacteria and the immune system
I watched as he shrank…not in size, but in hope. He never voiced it, but I could sense it—a belief that this struggle was supposed to be over, that he had traded one illness for another. The body he had already surrendered to was once again trying to negotiate.
“Chronic pouchitis”, that’s what it was eventually named. He needed stronger medications. Immunosuppressants. And lurking in the background was the ominous possibility of another surgery—perhaps even a permanent ileostomy.
Once more, we began speaking in “ifs.” If this treatment works… If this flare passes… If we can get through next week without another ER visit…
But through it all, he fought..not with loud proclamations or anger, but with a stubborn routine. With grit, that sought no applause. He packed his medications in a lunchbox. Brought his own food to get-togethers. Laughed when he could, and slept when he couldn’t.
I witnessed the toll it took on him, not just the pain, but the relief he thought he had rightfully earned after the surgery. The dream of closure, of moving forward.
And still, he rises each day, still tries, still eats carefully, lives cautiously, and loves deeply…even as his body narrows the margins.
📘 Diagnosis & Treatment
diagnosis:
– Medical history and physical exam
– Blood tests (to rule out other causes and assess inflammation)
– Stool tests (to identify infections and guide antibiotics)
– Endoscopy (to examine pouch and collect biopsy)
– Imaging (MRI or CT scan if needed for further evaluation)
Treatment:
Antibiotics:
– Most effective first-line treatment
– Symptoms often improve within 1–2 days
– Typical course lasts 10–14 days
– Longer courses or rotating antibiotics may be used for chronic pouchitis
Probiotics:
– May help prevent recurrence
– Often used as adjunctive therapy in long-term cases
surgery:
– Rarely, if chronic and unresponsive to treatment
– May require removal of the pouch and creation of a permanent ileostomy
Pouchitis is inflammation of the ileal pouch
a surgically created internal reservoir that replaces the rectum in people who’ve had their colon removed, typically due to ulcerative colitis. It can cause sudden digestive symptoms, including pain, urgency, and bowel dysfunction. Though often treated effectively with antibiotics, recurring cases may require long-term management or even surgical revision.
I know this is heavy, and I understand that the road ahead may feel like a tangle of loss and unanswered questions. But please hear this: you are not broken because you are hurting; you are not weak because you are afraid. You are living through something real, and survival itself is a kind of grace. You are allowed to struggle, you are allowed to hope, and you are allowed to not have all the answers today. Whatever comes next, you do not face it empty-handed; you carry every moment of love that shaped you, and that will always be enough to keep going.
🎀 Gifts to help With J-pouch
🏥 Everyday Comforts for Everyday Battles
Managing J-pouch often means needing a little extra help.
Sometimes it’s about restoring dignity, ease, or simply getting through the day with less pain.
These carefully chosen tools aren’t just items; they’re small bridges back to living.
This section is about finding practical support, never shame.
Bidet Bottle for Travel + Home – Soothing Relief When Wipes Just Make It Worse
When you’ve had J-pouch surgery, flare-ups like pouchitis make hygiene painful. This gentle-spray bidet bottle offers soothing, non-irritating cleansing during times of urgency, soreness, or inflammation. It’s portable, discreet, and far kinder than dry toilet paper—especially on days when you’re going 10+ times and your body’s already raw.
🌿 Paths to Healing Beyond the Map
Sometimes traditional medicine isn’t enough.
If you’re exploring gentle, alternative options to help with J-pouch,
you might find comfort in plant-based compounds like **CBD or CBG**.
*This section is not medical advice, just a door left open.*
USA Medical Gut Health Total Pack – Gentle Backup When Your Rewired System Flares
Pouchitis brings pain, urgency, and inflammation even after the colon is gone. This Gut Health Pack supports digestive balance with CBD and gut-soothing botanicals—offering a layer of calm when antibiotics and diet aren’t enough. It won’t stop a flare. But it might help reduce the frequency and severity of the fallout.
Need a Different Path Forward?
Every journey through grief looks different. Choose the next step that speaks to where you are now:
When You're Ready to Start Healing
Healing doesn’t mean forgetting.
It means finding small ways to carry your grief with strength and grace.
These are the stories, tools, and gentle steps to begin walking forward…at your own pace.
When You're Still in the Thick of It
Sometimes healing feels like a lie.
If you’re not ready to move on…if the pain still roars louder than the world wants to hear…this is the place where you’re allowed to feel it.
No sugarcoating. No pretending. Just truth.
When You're Holding on to Who’s Still Here
Grief reminds us to love louder.
If someone you love is still with you, this is your place to celebrate them, honor them, and create new memories while there’s still time.
Joy and sorrow can live side by side.