Grieving Lupus: When the Body Becomes Its Own Enemy
Grief with lupus rises and falls, watching someone you love lose battles inside their own skin, fighting a war that never fully ends.
This post blends real grief with grounded knowledge. It isn’t clinical. It isn’t distant. It’s meant to sit beside you—not above you. The story you’ll read is meant to reflect what so many feel when living through or witnessing this condition: confusion, exhaustion, and quiet forms of courage.
If what you read feels familiar, please speak with your doctor. Your pain deserves more than silence.
Some Days She Fought, Some Days She Hid from the Hurt
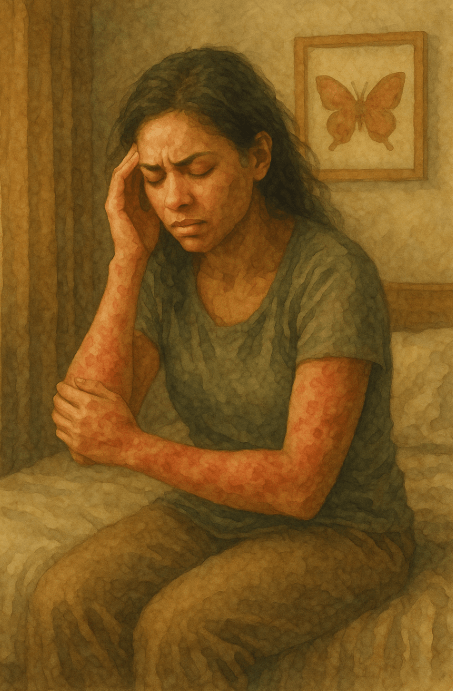
She never showed signs of illness… That was the first betrayal.
Her skin remained smooth, her eyes retained their brightness. So, when she spoke of her pain, people tilted their heads, suggesting yoga as a remedy.
She had tried yoga. Along with turmeric, gluten-free, dairy-free, and nightshade-free diets. She experimented with sleep schedules, stretching, and feigned happiness.
But lupus doesn’t care about good intentions.
It slipped in gradually. Aches that wandered, fatigue that defied any logical explanation, and rashes that appeared and vanished like fleeting shadows on her skin. Blood tests hinted at answers but provided little clarity. One doctor labeled it as stress, and another called it fibromyalgia. It wasn’t until her twelfth visit that someone finally said, “We think it’s lupus
🧠 Symptoms:
– Fatigue
– Fever
– Joint pain, stiffness, and swelling
– Butterfly-shaped rash across cheeks and nose
– Skin lesions triggered by sun exposure
– Fingers or toes turning white or blue with cold/stress (Raynaud’s)
– Shortness of breath
– Chest pain
– Headaches, confusion, memory loss
– Dry eyes
– Mouth sores
Even then, the word “think” was key. Lupus doesn’t always announce itself boldly. It masquerades as other conditions, lurking within lab results and partial symptoms. But deep down, she knew. She recognized it by its name.
Once it had a name, the heartbreak began…not because it was deadly, but because it was unending.
Every flare became a gamble. Would it target her joints, her skin, her lungs, or her kidneys? Would today be a good day, or would sunlight feel like daggers against her cheeks?
We learned the patterns: the medications, the well-known steroid moon face, the immune suppressants, the anxiety that encompassed every sneeze in a crowded setting.
Complications:
– **Kidneys**: lupus nephritis, kidney failure (leading cause of death)
– **Brain and CNS**: strokes, seizures, memory problems, behavioral changes
– **Blood and vessels**: anemia, clotting issues, inflammation of blood vessels
– **Lungs**: pleuritis, pneumonia, bleeding
– **Heart**: myocarditis, pericarditis, increased risk of heart attack
– **Other**:
– Increased infection risk (from disease and treatment)
– Higher cancer risk (though small)
– Osteonecrosis (bone tissue death)
– Pregnancy complications (e.g., miscarriage, preeclampsia)
Causes:
– Autoimmune response triggered by genetic and environmental factors
– Environmental triggers may include:
– Sunlight (UV exposure)
– Infections
– Certain medications (e.g., anti-seizure drugs, antibiotics, blood pressure meds)
– Most causes remain unknown in specific cases
Some days, she fought back. She took her medication, completed her stretches, and tackled her day with coffee, courage, and a to-do list.
Other days, she withdrew. She silenced her phone, lay in bed, staring at the ceiling, as even the act of blinking felt like an act of defiance.
She was not weak. She was engaged in a battle against her own immune system, against her own body, and against a world that kept questioning why she hadn’t simply “gotten over it.”
But she never surrendered…
Not once…
Even during those moments when tears fell quietly in the shower, so I wouldn’t hear. Even when she canceled plans that excited her for weeks. Even when she smiled and said, “I’m fine,” while her body screamed the opposite.
She’s still here. Still fighting. Still experiencing flares but also still living. While lupus may not be curable, she does not view herself as its victim. She is its survivor, its storm-walker, its response to the question: What if pain didn’t triumph?
Risk Factors:
– Sex: more common in women
– Age: most often diagnosed between ages 15 and 45
– Race: higher prevalence in Black, Hispanic, and Asian individuals
– Family history of autoimmune disease
She didn’t succumb to lupus…she learned to coexist with it, even when it tried to silence her every step.
📘 Diagnosis & Treatment
diagnosis:
– No single definitive test—diagnosis is based on clinical evaluation + labs
– Blood and urine tests:
– Complete blood count (CBC)
– ANA (Antinuclear Antibody Test)
– ESR and CRP (inflammation markers)
– Kidney/liver function tests
– Urinalysis (protein or blood in urine)
– More-specific antibody panels (anti-dsDNA, anti-Smith)
– Imaging:
– Chest X-ray or echocardiogram (for heart/lung involvement)
– Biopsies:
– Kidney or skin samples to determine organ damage and direct treatment
treatment:
– **NSAIDs**: for joint pain and inflammation (e.g., ibuprofen, naproxen)
– **Antimalarials**: hydroxychloroquine (Plaquenil)—baseline treatment for many
– **Corticosteroids**: high-dose for acute flares or organ involvement (e.g., prednisone)
– **Immunosuppressants**: for severe disease (e.g., azathioprine, methotrexate, mycophenolate)
– **Biologics**: belimumab (Benlysta), rituximab—target immune system proteins
– **Newer agents**: voclosporin, anifrolumab (under study or selective use)
– Treatment plans are tailored and adjusted based on disease severity and organ involvement
Self Care:
– Regular medical checkups—even during remission
– Sun protection (SPF 55+, hats, long sleeves)
– Moderate, regular exercise
– No smoking (exacerbates cardiovascular and autoimmune complications)
– Balanced diet; restrict salt if hypertensive or protein if kidneys are affected
– Vitamin D and calcium supplements (especially with corticosteroid use)
– Track flares and symptoms to assist with treatment adjustment
alternative therapies:
– DHEA (hormonal supplement, may reduce flares—acne is a side effect)
– Fish oil (omega-3 anti-inflammatory support)
– Acupuncture (for chronic muscle pain)
– Use cautiously—always with physician oversight
coping and support:
– Mental health care is essential: depression, anxiety, and grief are common
– Journaling, meditation, music, and creative outlets help manage emotional burden
– Join support groups—either local or online—for shared experiences
– Educate family and friends so they understand the invisible nature of the illness
– Communicate clearly about your needs during flares and fatigue days
I know this is heavy, and I understand that the road ahead may feel like a tangle of loss and unanswered questions. But please hear this: you are not broken because you are hurting; you are not weak because you are afraid. You are living through something real, and survival itself is a kind of grace. You are allowed to struggle, you are allowed to hope, and you are allowed to not have all the answers today. Whatever comes next, you do not face it empty-handed; you carry every moment of love that shaped you, and that will always be enough to keep going.
🎀 Gifts to help With Lupus
🏥 Everyday Comforts for Everyday Battles
Managing Lupus often means needing a little extra help.
Sometimes it’s about restoring dignity, ease, or simply getting through the day with less pain.
These carefully chosen tools aren’t just items; they’re small bridges back to living.
This section is about finding practical support, never shame.
UV-Blocking Sun Hoodie – Shielding Skin from a Flare That Needs No Invitation
Sun exposure can trigger lupus flares—turning a simple walk outside into a risk. This lightweight, breathable UV-protective hoodie offers full coverage without overheating, protecting sensitive skin while still feeling soft enough for daily wear. It’s more than sun protection. It’s a preemptive shield when the immune system’s waiting for a reason to ignite.
🌿 Paths to Healing Beyond the Map
Sometimes traditional medicine isn’t enough.
If you’re exploring gentle, alternative options to help with Lupus,
you might find comfort in plant-based compounds like **CBD or CBG**.
*This section is not medical advice, just a door left open.*
USA Stress Total Pack – Support for a Body Fighting Itself Every Day
Lupus attacks everything—joints, energy, sleep, mood. This Total Pack offers CBD, inflammation relief, and gentle nervous system support to help the body breathe between battles. It won’t stop the flares. But it may soften the edges. For the days when even rest feels like effort.
Need a Different Path Forward?
Every journey through grief looks different. Choose the next step that speaks to where you are now:
When You're Ready to Start Healing
Healing doesn’t mean forgetting.
It means finding small ways to carry your grief with strength and grace.
These are the stories, tools, and gentle steps to begin walking forward…at your own pace.
When You're Still in the Thick of It
Sometimes healing feels like a lie.
If you’re not ready to move on…if the pain still roars louder than the world wants to hear…this is the place where you’re allowed to feel it.
No sugarcoating. No pretending. Just truth.
When You're Holding on to Who’s Still Here
Grief reminds us to love louder.
If someone you love is still with you, this is your place to celebrate them, honor them, and create new memories while there’s still time.
Joy and sorrow can live side by side.