Grieving Obstructive Lung Disease: When Air Itself Becomes the Enemy
Grief tied to obstructive lung disease builds with every shallow breath—watching someone fight invisible walls inside their own chest.
This post blends real grief with grounded knowledge. It isn’t clinical. It isn’t distant. It’s meant to sit beside you—not above you. The story you’ll read is meant to reflect what so many feel when living through or witnessing this condition: confusion, exhaustion, and quiet forms of courage.
If what you read feels familiar, please speak with your doctor. Your pain deserves more than silence.
He Gasped for Air While I Gasped for Hope
He never liked asking for help. Not when his knees gave out. Not when his hearing began to fade. And certainly not when the deep, guttural coughing started…an unsettling sound that seemed to rattle the walls and linger in the silence that followed.
He insisted it was just allergies. He claimed the house was too dusty. He said he’d been smoking since he was fifteen and had grown accustomed to it.
But no one truly gets used to drowning on dry land.
The diagnosis arrived later: Chronic Obstructive Lung Disease. A slow thief, it takes its toll gradually, stealing just a little more breath each year.
They reassured us that it was manageable…that if he quit smoking…and he did, white-knuckled and proud; if he took his medications, engaged in rehabilitation, and stayed ahead of flare-ups, perhaps he could preserve what lung function remained.
🧠 Symptoms:
– Shortness of breath, especially with exertion
– Chronic cough with mucus (clear, yellow, green, or white)
– Wheezing or whistling breath sounds
– Chest tightness
– Fatigue or low energy
– Recurrent respiratory infections
– Unintentional weight loss (in later stages)
– Swelling in ankles, feet, or legs
– Exacerbations: symptom flare-ups triggered by cold air, infections, or pollutants
Yet “manageable” didn’t equate to livable, especially when the walk to the kitchen felt like a marathon, when laughter ended in choking, and when the air betrayed him even at rest.
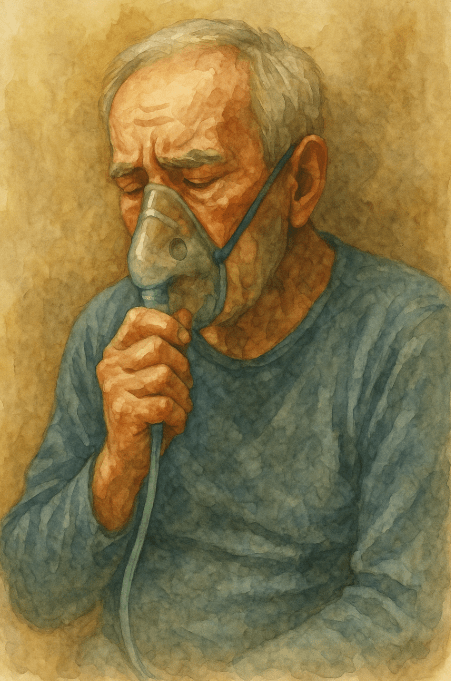
I watched him transform into a different man: measured, cautious. Every movement became a negotiation with his lungs. He started to use terms like exacerbation, sputum, and spirometry…words that had no place in his vocabulary before disease had claimed his space.
We devised a plan: pulmonary rehab, inhalers in every drawer, steroids for flare-ups, and a list of ER signs taped to the fridge like a silent prayer.
But still, the flare-ups came…
In the middle of the night. During dinner. In the midst of conversation.
I’d hear him wheezing before I could see him, eyes widened, hands pressed against the counter as if wrestling with gravity. And perhaps he was.
Complications:
– Respiratory infections (e.g., flu, pneumonia)
– Heart disease and arrhythmias
– Lung cancer
– Pulmonary hypertension
– Depression and anxiety
– Acute respiratory failure during exacerbations
Causes:
– Long-term exposure to lung irritants:
– Cigarette smoke (primary cause)
– Cigar and pipe smoke
– Air pollution
– Workplace exposure to dust, fumes, or chemicals
– Indoor smoke from cooking/heating (especially in homes with poor ventilation)
– Genetic condition: Alpha-1-antitrypsin deficiency (rare)
He gasped for air. And I, I gasped for hope.
I clung to the belief that the oxygen tanks would suffice, that we had more time together, that I wouldn’t have to learn the sound of his struggle when he could no longer catch his next breath.
He despised the weakness, loathed the noise of his own lungs. Yet he never relinquished his dignity.
Even as his voice faded. Even when the stairs became insurmountable. Even when the world seemed to close in around him.
He still expressed gratitude. He still watched the news. He still attempted to smile, despite the haze of carbon dioxide retention and sleepless nights.
In those final days, I found myself sitting beside him more often. Not because I had the right words to say, but because the silence was more bearable than pretending I could rescue him.
“Memory doesn’t die all at once. It drips. It slips. Until only love is left—and even that forgets its name.”.
Risk Factors:
– Smoking (active or secondhand exposure)
– Occupational exposure to fumes or dust
– Childhood respiratory infections
– Asthma or airway hyperresponsiveness
– Family history of COPD
– Older age
– Low socioeconomic status (linked to higher exposure and less care access)
📘 Diagnosis & Treatment
diagnosis:
– Clinical history and physical exam
– Pulmonary function tests (especially spirometry)
– Arterial blood gas tests (oxygen and carbon dioxide levels)
– Chest X-ray or CT scan
– Pulse oximetry
– AAT testing (if under 45 or with family history)
treatment:
smoking cessation:
– Most important step to slow disease progression
– Medications, nicotine replacement, counseling, support groups
medications:
bronchodilators:
– Short-acting (e.g., albuterol)
– Long-acting (e.g., tiotropium, salmeterol)
inhaled_steroids:
– Fluticasone, budesonide (for frequent exacerbations)
combination_inhalers:
– Bronchodilator + steroid or multiple bronchodilators
oral_steroids:
– Used for acute exacerbations (short-term)
phosphodiesterase-4_inhibitor:
– Roflumilast (for severe COPD with chronic bronchitis)
theophylline:
– Older medication, less preferred due to side effects
antibiotics:
– Used during infections or exacerbations
therapies:
– Oxygen therapy (if oxygen levels are low)
– Pulmonary rehabilitation (exercise + education + counseling)
– Noninvasive ventilation (e.g., BiPAP) for severe cases
surgical options:
– Lung volume reduction surgery
– Endobronchial valve placement
– Bullectomy (removal of large air sacs)
– Lung transplant (in advanced cases)
lifestyle and prevention:
– Get annual flu and pneumonia vaccines, as well as COVID-19 and RSV vaccines
– Avoid smoke, air pollution, and other triggers
– Use controlled breathing and mucus-clearing techniques
– Eat a healthy diet and maintain weight
– Practice gentle but consistent physical activity
– Keep regular appointments to track disease progression
coping and support:
– Depression and anxiety are common—seek mental health care if needed
– Join COPD support groups or pulmonary rehab programs
– Educate family and caregivers about COPD triggers and emergency plans
– Create a home environment with good air quality and accessible equipment
I know this is heavy, and I understand that the road ahead may feel like a tangle of loss and unanswered questions. But please hear this: you are not broken because you are hurting; you are not weak because you are afraid. You are living through something real, and survival itself is a kind of grace. You are allowed to struggle, you are allowed to hope, and you are allowed to not have all the answers today. Whatever comes next, you do not face it empty-handed; you carry every moment of love that shaped you, and that will always be enough to keep going.
🎀 Gifts to help With Obstructive Lung Disease
🏥 Everyday Comforts for Everyday Battles
Managing Obstructive Lung Disease often means needing a little extra help.
Sometimes it’s about restoring dignity, ease, or simply getting through the day with less pain.
These carefully chosen tools aren’t just items; they’re small bridges back to living.
This section is about finding practical support, never shame.
Portable Pulse Oximeter – Data for Lungs That Lie About How Much Air They Have
In obstructive lung disease, you can feel like you’re breathing—but still be starved of oxygen. This fingertip pulse oximeter gives real-time readings of O₂ saturation and pulse rate, helping patients track drops during walking, climbing, or flare-ups. It’s a tiny tool that offers clarity when lungs say “fine” but blood says “not enough.”
🌿 Paths to Healing Beyond the Map
Sometimes traditional medicine isn’t enough.
If you’re exploring gentle, alternative options to help with Obstructive Lung Disease,
you might find comfort in plant-based compounds like **CBD or CBG**.
*This section is not medical advice, just a door left open.*
USA Medical Total Support Pack – Reinforcement for Lungs That Trap More Than Air
COPD rooted in obstruction builds slowly—damaging bronchioles, exhausting the diaphragm, and choking out rest. This Total Pack provides CBD, calming adaptogens, and gentle immune support to help the body recover between flare-ups. It doesn’t expand lung capacity. But it helps steady the system behind it.
Need a Different Path Forward?
Every journey through grief looks different. Choose the next step that speaks to where you are now:
When You're Ready to Start Healing
Healing doesn’t mean forgetting.
It means finding small ways to carry your grief with strength and grace.
These are the stories, tools, and gentle steps to begin walking forward…at your own pace.
When You're Still in the Thick of It
Sometimes healing feels like a lie.
If you’re not ready to move on…if the pain still roars louder than the world wants to hear…this is the place where you’re allowed to feel it.
No sugarcoating. No pretending. Just truth.
When You're Holding on to Who’s Still Here
Grief reminds us to love louder.
If someone you love is still with you, this is your place to celebrate them, honor them, and create new memories while there’s still time.
Joy and sorrow can live side by side.