When Fear and Ritual Replace Freedom Grieving: Obsessive-Compulsive Disorder (OCD)
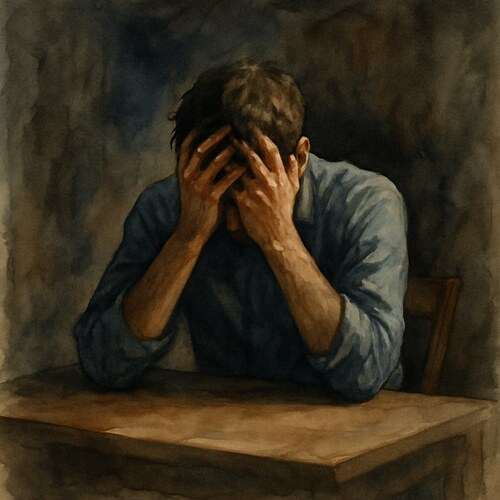
Grief with OCD isn’t about quirks; it’s about losing time, joy, and peace to battles fought behind locked doors and whispered fears.

This post blends real grief with grounded knowledge. It isn’t clinical. It isn’t distant. It’s meant to sit beside you—not above you. The story you’ll read is meant to reflect what so many feel when living through or witnessing this condition: confusion, exhaustion, and quiet forms of courage.
If what you read feels familiar, please speak with your doctor. Your pain deserves more than silence.
I Lost Him to the Rituals He Couldn’t Break Free From
At first, it appeared to be a matter of discipline. He always kept himself clean and was consistently early. His pens were meticulously arranged by color, each label facing the same direction, like tiny soldiers in a conflict he unknowingly enlisted in.
People referred to him as organized. They often expressed their envy of his focus, remarking that he must sleep well, knowing everything was neat and in its place.
But he didn’t sleep…
He counted steps, tiles, breaths. Each night, he felt compelled to turn the light on and off an even number of times before bed—not for comfort, but because if he didn’t, his mother would die. She’d been gone for six years.
This wasn’t superstition; it was pure terror…
That’s where people often miss the mark…
OCD is not just about quirky habits or alphabetized bookshelves. It manifests as bloodied knuckles from over-washing, as burnt dinners because he couldn’t stop checking the stove, as hours wasted agonizing over a single locked door, still doubting if it was truly shut.
I witnessed his slow spiral…
🧠 Symptoms:
obsessions:
– Intrusive, distressing thoughts, urges, or images
– Fear of contamination, dirt, or germs
– Doubts about having done something right (e.g., locking doors)
– Intense need for symmetry or order
– Thoughts of harming others or oneself
– Unwanted taboo thoughts (e.g., sexual, religious)
compulsions:
– Repetitive acts to neutralize or prevent distress
– Excessive hand-washing or cleaning
– Rechecking locks, appliances, or steps repeatedly
– Counting patterns or doing tasks in a specific order
– Repeating words or prayers silently
– Arranging items “just right”
– Seeking reassurance repeatedly
severity and onset:
– Often begins in childhood, teen, or early adult years
– Can worsen during stress, life changes, or trauma
– May fluctuate in intensity over time
– Can become disabling if untreated
At first, it was about hygiene, then it morphed into fears of contamination, and eventually turned inward—he became a prisoner of his own mind.
He avoided physical contact. He claimed he didn’t trust his hands and worried he might have picked up “something” while out. He would say, “I don’t want to hurt anyone.”
He apologized more than necessary…about thoughts he couldn’t control, about obsessions that replayed in his mind like shards of broken glass caught in a blender. He asked the same question repeatedly: “Are you sure I didn’t hurt you? Are you sure? Are you sure?”
I assured him every time. Yet, each time, he looked at me as if the truth didn’t quite fit.
The compulsions weren’t actually comforting; they were like cages. False promises that maybe this time, if he did it just right, the chaos would fade away.
He tried therapy, Exposure Response Prevention. He held his trembling hands still and worked to sit with his discomfort. He tried medication. He tried silence.
Complications:
– Time-consuming rituals that interfere with work/school
– Skin damage from over-washing
– Social withdrawal and relationship strain
– Depression and suicidal thoughts
– Poor quality of life
Causes:
– Biology: Changes in brain chemistry or function
– Genetics: Family history increases risk
– Learned behaviors: May develop through observation or habit
– No single known cause—often multifactorial
But OCD is not a linear journey. It doesn’t quietly exit; it simply hides. It waits. It sleeps, then it awakens again.
Eventually, he stopped coming to dinner. He claimed he needed to stay home, insisting he couldn’t leave until he “finished” whatever was holding him captive. When I asked what needed finishing, he had no answer. He just closed the door.
I loved him deeply…still do. Yet, I lost him to an invisible war, a battle where the enemy was locked within his own mind, and it wielded his voice.
Risk Factors:
– Family history of OCD or related conditions
– Stressful or traumatic life events
– Co-occurring mental health disorders (anxiety, depression, substance abuse, tic disorders)
He didn’t want to repeat things; he had to. Each ritual that calmed the storm took a little more of him with it.
📘 Diagnosis & Treatment
diagnosis:
– Psychological evaluation (self-report + clinical interview)
– Rule out other mental health disorders or physical causes
– Consider differential diagnoses (e.g., OCD vs. perfectionism vs. schizophrenia)
– May involve family input and behavioral history
treatment:
psychotherapy:
– Cognitive Behavioral Therapy (CBT) with Exposure and Response Prevention (ERP)
– ERP exposes patient to feared thoughts and teaches resisting compulsions
– Highly effective but requires consistency and support
medications:
– SSRIs: fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), sertraline (Zoloft)
– Tricyclic antidepressant: clomipramine (Anafranil)
– High doses may be needed; takes weeks to months for full effect
– Monitor for side effects and possible suicidal thoughts (especially in youth)
advanced options:
– Intensive outpatient or residential programs
– Transcranial Magnetic Stimulation (TMS)
– Deep Brain Stimulation (DBS) for treatment-resistant cases
lifestyle and self management:
– Practice learned coping techniques (ERP exercises)
– Stick to medication and therapy schedule
– Monitor early warning signs of relapse
– Avoid triggers when possible or address them with support
– Build a calm daily routine and reduce stress
coping_and_support:
– Join support groups for OCD
– Educate loved ones to reduce stigma and misunderstanding
– Engage in physical activity, hobbies, and mindfulness
– Use stress-relief tools like breathing, meditation, or yoga
– Avoid isolation—stay engaged with work, school, or community
I know this is heavy, and I understand that the road ahead may feel like a tangle of loss and unanswered questions. But please hear this: you are not broken because you are hurting; you are not weak because you are afraid. You are living through something real, and survival itself is a kind of grace. You are allowed to struggle, you are allowed to hope, and you are allowed to not have all the answers today. Whatever comes next, you do not face it empty-handed; you carry every moment of love that shaped you, and that will always be enough to keep going.
🎀 Gifts to help With Obsessive-compulsive disorder
🏥 Everyday Comforts for Everyday Battles
Managing Obsessive-Compulsive Disorder often means needing a little extra help.
Sometimes it’s about restoring dignity, ease, or simply getting through the day with less pain.
These carefully chosen tools aren’t just items; they’re small bridges back to living.
This section is about finding practical support, never shame.
Grounding Tactile Stone – A Quiet Anchor When the Ritual Isn’t an Option
When OCD spikes, your brain demands action—wash again, check again, count again. This grounding stone gives your hands something else to do: traceable grooves, soothing textures, and subtle sensory input to help redirect the compulsion without feeding it. Small enough to keep in a pocket. Quiet enough to carry without shame.
🌿 Paths to Healing Beyond the Map
Sometimes traditional medicine isn’t enough.
If you’re exploring gentle, alternative options to help with Obsessive-Compulsive Disorder,
you might find comfort in plant-based compounds like **CBD or CBG**.
*This section is not medical advice, just a door left open.*
USA Medical Stress Relief Total Pack – Nervous System Calm for the Mind That Won’t Let Go
OCD doesn’t give breaks—it cycles endlessly, especially when stress and fatigue set in. This Total Pack blends CBD, calming botanicals, and nervous system support to help reduce reactivity and emotional overload. It won’t silence intrusive thoughts. But it may soften how loudly they demand a response.
Need a Different Path Forward?
Every journey through grief looks different. Choose the next step that speaks to where you are now:
When You're Ready to Start Healing
Healing doesn’t mean forgetting.
It means finding small ways to carry your grief with strength and grace.
These are the stories, tools, and gentle steps to begin walking forward…at your own pace.
When You're Still in the Thick of It
Sometimes healing feels like a lie.
If you’re not ready to move on…if the pain still roars louder than the world wants to hear…this is the place where you’re allowed to feel it.
No sugarcoating. No pretending. Just truth.
When You're Holding on to Who’s Still Here
Grief reminds us to love louder.
If someone you love is still with you, this is your place to celebrate them, honor them, and create new memories while there’s still time.
Joy and sorrow can live side by side.